Difference Between Gas Pain and Heart Attack: Could You Be Mistaking a Burp for an Emergency?
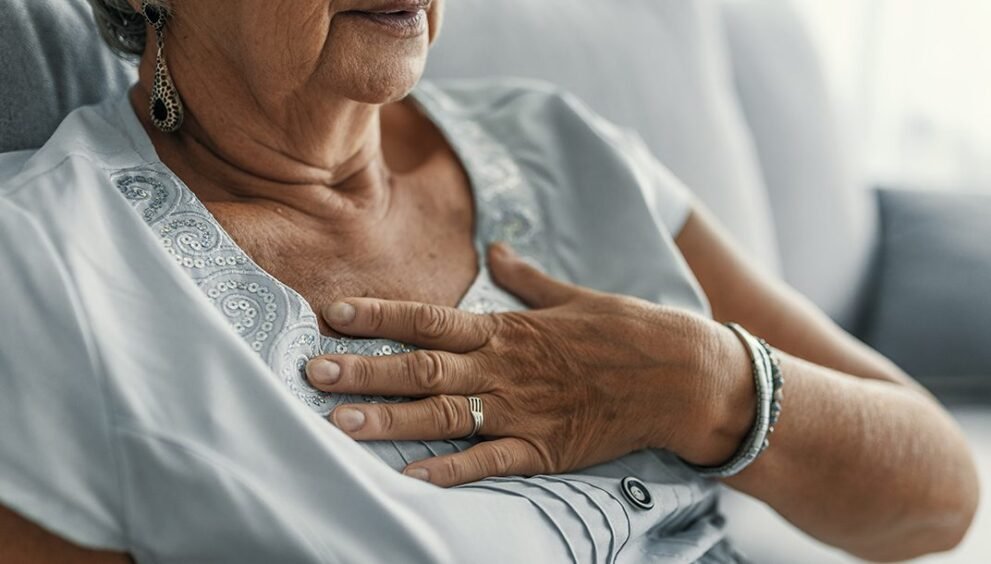
The difference between gas pain and heart attack can feel like a blurry line when discomfort strikes unexpectedly. Imagine sitting down after a big meal, feeling a sharp twinge in your chest or a bloated ache in your abdomen, and wondering, “Is this just gas, or something serious?” For Americans, where heart disease remains a leading cause of death, distinguishing these sensations is critical. Misjudging symptoms could mean brushing off a life-threatening emergency or panicking over something as simple as indigestion. This blog dives into the nuances of these conditions, offering clarity for anyone who’s ever second-guessed their symptoms.
Understanding the Basics
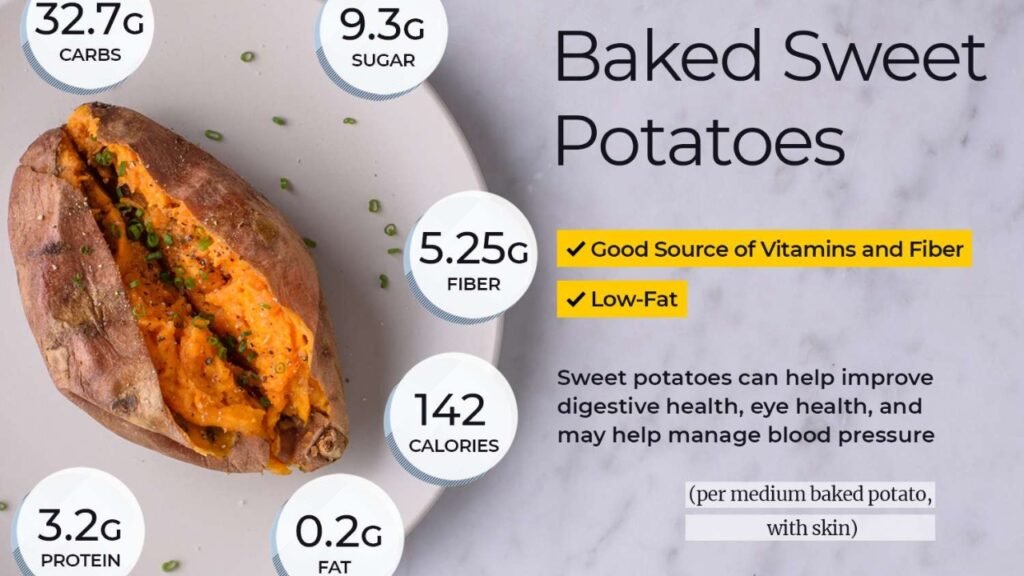
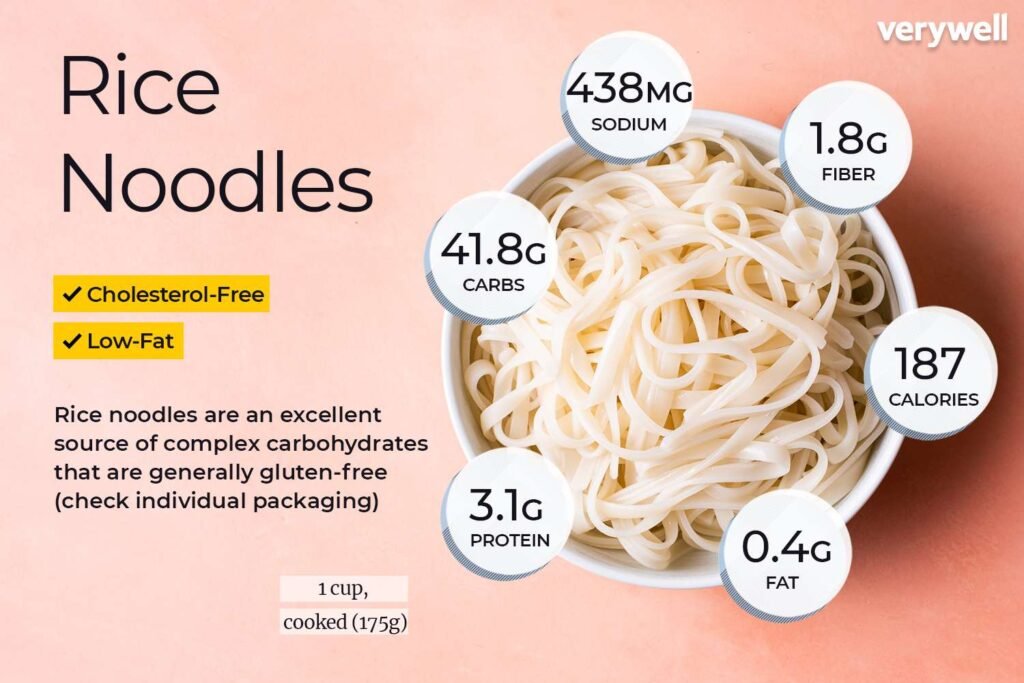
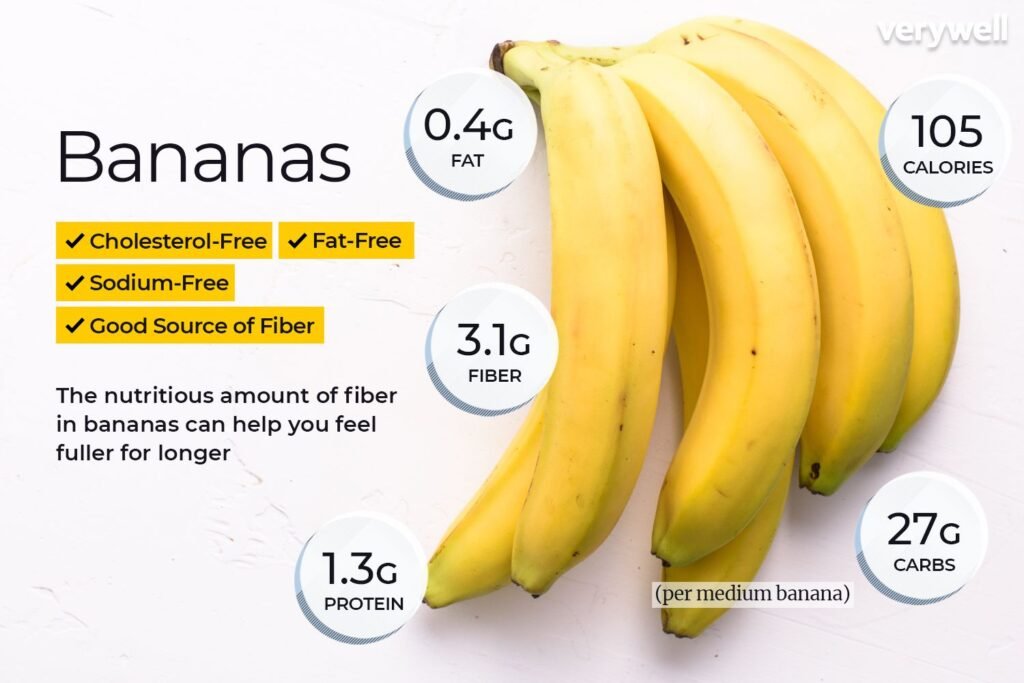
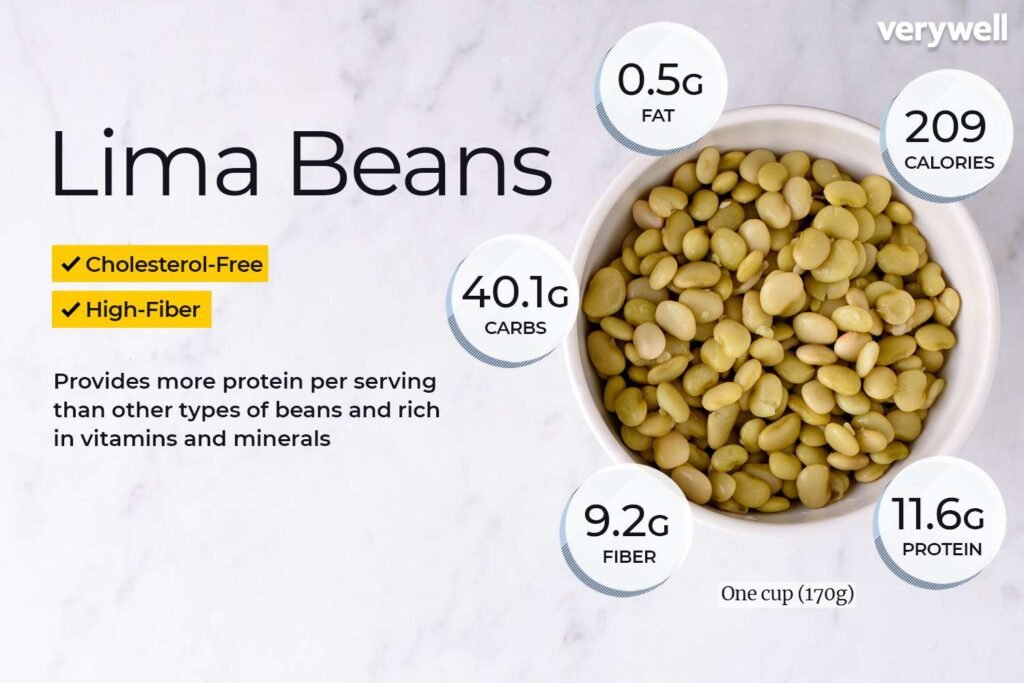
Difference between gas pain and heart attack arises when air gets trapped in your digestive system, often due to swallowed air, food breakdown, or dietary choices. It’s a common issue, especially after eating gas-producing foods like beans, broccoli, or dairy for the lactose-intolerant. The discomfort typically manifests as bloating, cramping, or sharp jabs in the abdomen. Sometimes, this pain radiates upward, mimicking chest discomfort, which muddies the waters when comparing it to heart-related issues. For many, gas pain is fleeting, resolving with movement, a burp, or over-the-counter remedies like simethicone.
However, the intensity can catch you off guard. On Reddit, users often describe gas pain as “a stabbing sensation” that feels alarming but subsides after passing gas or changing positions. One user shared, “I thought I was having a heart attack once, but it was just trapped gas from eating too much chili!” This highlights how diet and digestion play massive roles in these symptoms, yet the overlap with more serious conditions sparks confusion.
What Is a Heart Attack?
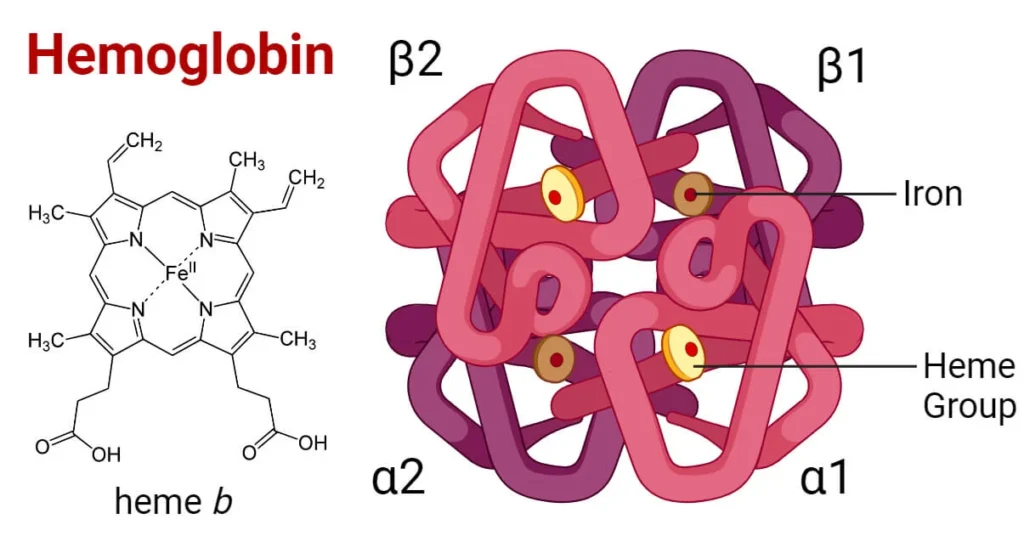
A heart attack, or myocardial infarction, occurs when blood flow to the heart is blocked, often by a clot in a coronary artery. This deprives the heart muscle of oxygen, leading to damage or death of tissue if untreated. Symptoms vary widely, which complicates self-diagnosis. Classic signs include chest pain or pressure, often described as a heavy, squeezing sensation. Unlike gas pain, heart attack symptoms may spread to the arms, jaw, neck, or back and persist beyond a few minutes.
Importantly, heart attacks don’t always announce themselves dramatically. Some Reddit users recount “silent” symptoms, like mild discomfort or fatigue, mistaken for indigestion. One commenter noted, “My dad thought his chest tightness was from eating tacos, but it was his heart.” This variability underscores why understanding the difference between gas pain and heart attack is so vital, especially for Americans over 40, who face higher risks.
Difference Between Gas Pain and a Heart Attack: Key Distinctions
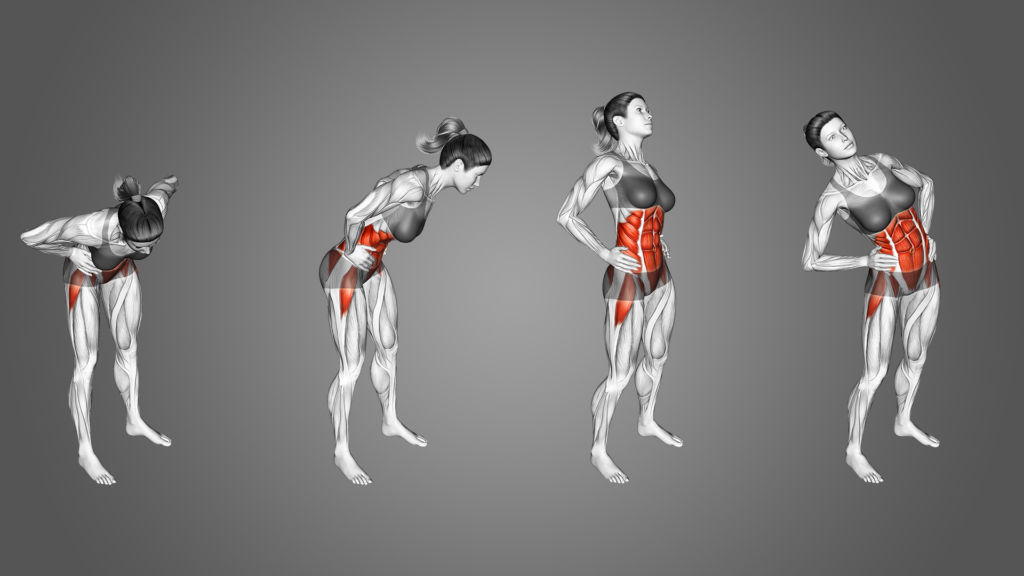
One key to distinguishing gas pain from a heart attack lies in where and how the pain feels. Gas pain typically centers in the abdomen, though it can radiate to the chest, creating confusion. The sensation is often sharp, crampy, or bloated, tied to digestive processes. Moving around, passing gas, or having a bowel movement usually eases it. In contrast, heart attack pain often starts in the chest and feels like pressure, fullness, or squeezing. It’s less likely to shift with body position or digestion.
Moreover, heart attack pain tends to spread. Dr. Sarah Thompson, a cardiologist quoted in a recent health journal, explains, “Chest pain that radiates to the left arm, jaw, or back is a red flag for a cardiac event, whereas gas pain stays more localized to the digestive tract.” This distinction is crucial, yet not foolproof, as some heart attacks present with vague abdominal discomfort, especially in women or older adults.
Accompanying Symptoms
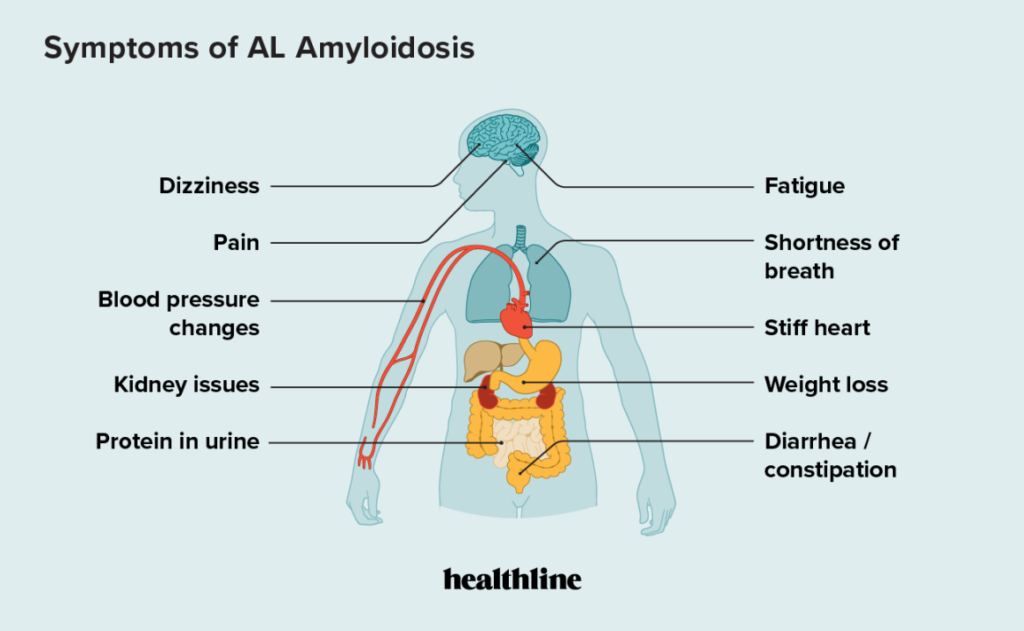
Another way to parse gas pain from a heart attack is by noting what else you’re feeling. Gas pain often comes with bloating, burping, or flatulence—clear digestive clues. You might feel fine otherwise, with no systemic symptoms. Heart attacks, however, frequently bring companions like shortness of breath, nausea, sweating, or dizziness. These signs point to a body under stress, not just a stomach processing last night’s tacos.
Reddit discussions echo this. One user described gas pain as “annoying but isolated,” while another shared a heart attack scare involving “sweating buckets and feeling like I couldn’t breathe.” These stories highlight how systemic symptoms tilt the scales toward a cardiac concern, urging caution if you’re unsure.
Timing and Triggers
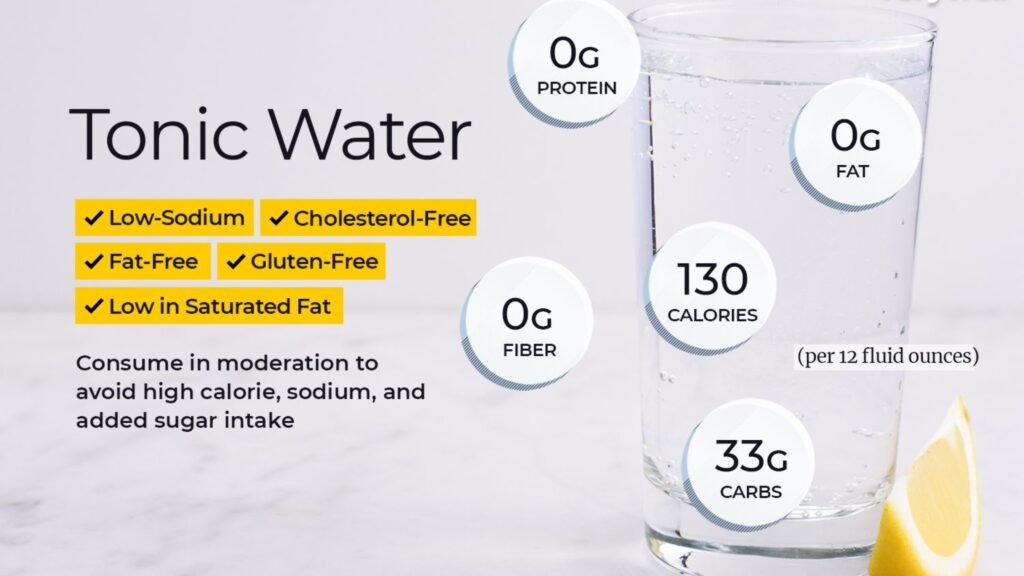
When symptoms hit can also clarify the difference. Gas pain often ties to meals, especially heavy, spicy, or fibrous ones. Eating too fast or drinking carbonated beverages can exacerbate it. The discomfort may flare up soon after eating and fade within hours. Heart attack symptoms, however, may strike without an obvious trigger, like during rest or stress. They tend to last longer—beyond 10-15 minutes—and don’t resolve with antacids or belching.
Interestingly, some Reddit users mention mistaking early heart attack signs for indigestion because they ate recently. One wrote, “I popped Tums for chest pain after pizza, but it kept getting worse—turned out to be my heart.” This overlap in timing shows why paying attention to persistence and unrelated triggers matters.
Risk Factors to Consider
Almost everyone experiences gas pain at some point. Certain habits, like eating too quickly, chewing gum, or consuming trigger foods, increase the likelihood. Conditions like irritable bowel syndrome (IBS) or lactose intolerance can make it a recurring issue. Americans, with diets high in processed foods and sodas, may notice frequent bloating or cramping, as these disrupt gut balance. Stress also plays a role, slowing digestion and trapping gas.
However, gas pain alone doesn’t signal deeper health problems unless it’s chronic or paired with symptoms like weight loss or blood in the stool. For most, it’s a benign nuisance, manageable with dietary tweaks or over-the-counter aids.
Who’s at Risk for a Heart Attack?
Heart attack risk, conversely, hinges on more serious factors. Age, family history, smoking, high cholesterol, hypertension, diabetes, and obesity top the list. In the U.S., heart disease kills about 1 in 4 people, with men over 45 and women over 55 facing higher odds. Lifestyle factors, like a sedentary routine or poor diet, compound the danger. Stress and even sudden exertion, like shoveling snow, can trigger an event in at-risk individuals.
Reddit threads often mention regret over ignored risks. One user shared, “I’m 50, overweight, and shrugged off chest pain as gas—big mistake.” Knowing your personal risk—through checkups or family history—can guide how seriously you take symptoms.
When to Seek Help
Most gas pain resolves on its own. Simple fixes like walking, drinking water, or taking an antacid often do the trick. Over-the-counter meds like Gas-X or dietary changes, like cutting back on beans or dairy, can prevent recurrences. If the pain is frequent or severe, though, it might point to issues like acid reflux, food intolerances, or IBS, warranting a doctor’s visit.
Heart Attack: When to Act Fast
For heart attacks, time is muscle. If chest pain lasts more than 10 minutes, spreads, or comes with sweating, nausea, or breathlessness, call 911 immediately. Even if you’re unsure, it’s better to err on the side of caution. Women, in particular, may experience atypical symptoms like fatigue or back pain, which Reddit users often mention being dismissed until it’s critical.
The American Heart Association stresses acting fast: “Every minute delays treatment, more heart damage occurs.” Don’t wait for symptoms to “go away” or assume it’s just gas—emergency rooms can sort it out safely.
Practical Tips for Clarity
To avoid confusion, keep a mental checklist. If the pain ties to eating, eases with movement, or feels digestive, it’s likely gas. If it’s persistent, spreads, or brings systemic symptoms, treat it as urgent. Monitor your diet to reduce gas triggers, and know your heart health risks through regular checkups. Simple tools like a food diary or tracking symptoms can help spot patterns, giving you confidence in what your body’s saying.
For peace of mind, consider over-the-counter aids for gas or a cardiologist consultation if you’re high-risk. Reddit users often suggest keeping antacids handy but warn against relying on them for recurring chest pain—a smart balance of preparedness and vigilance.
Final Thoughts
The difference between gas pain and heart attack isn’t just academic—it’s a matter of life and limb. While a burp might signal relief from a spicy meal, lingering chest pressure could demand urgent action. By understanding where pain originates, what accompanies it, and how your risks stack up, you can navigate these moments with clarity. For Americans juggling busy lives and varied diets, this knowledge is power. So, the next time discomfort strikes, pause, assess, and act wisely—your gut (or heart) will thank you.