Navigating the Swallowing Struggle: Your Guide to the Dysphagia Diet
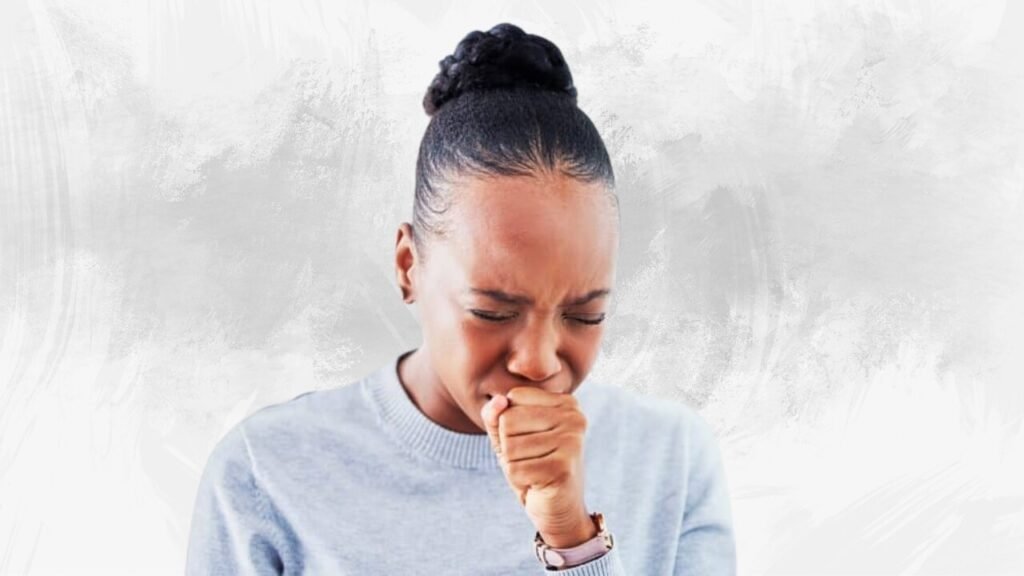
Do you or someone you adore struggle with swallowing? Does every meal feel like a potential hazard, filled with anxiety about choking or food getting stuck? If so, you’re probably familiar with the term dysphagia diet. This isn’t just a trendy food fad; it’s a carefully structured eating plan designed to help individuals with swallowing difficulties (dysphagia) eat safely and comfortably, improving their quality of life and preventing serious complications. This guide will explore the complexities of the dysphagia diet, providing the information you need to understand and implement it effectively.
Understanding Dysphagia: More Than Just Trouble Swallowing
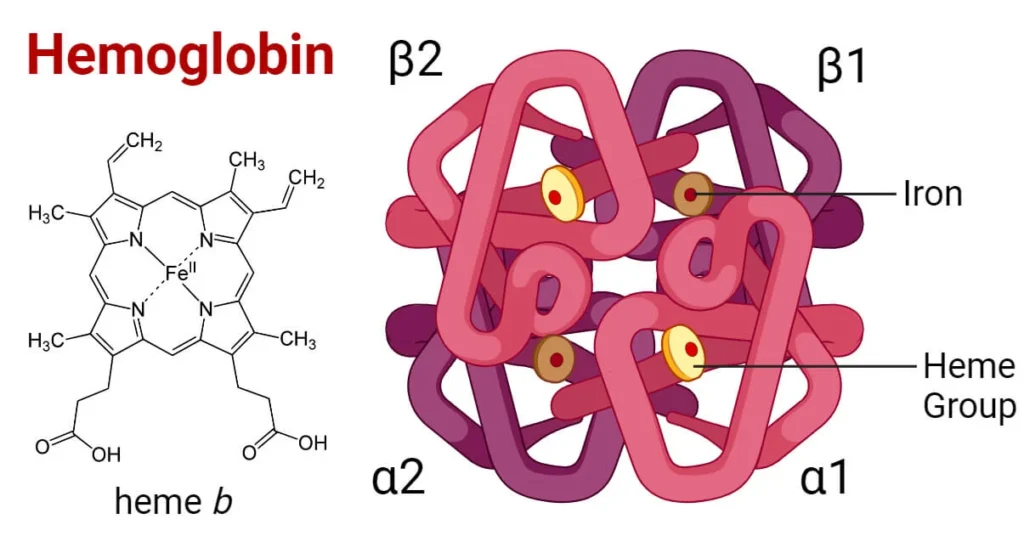
Dysphagia, at its core, means difficulty swallowing. However, the underlying causes and severity of dysphagia can vary widely. It can stem from neurological conditions like stroke, Parkinson’s disease, or multiple sclerosis; structural abnormalities in the mouth or esophagus; or even age-related changes in muscle strength and coordination. Therefore, understanding the specific cause of dysphagia is crucial for tailoring the most appropriate diet.
Dysphagia isn’t just about discomfort; it poses significant health risks. Aspiration, where food or liquid enters the lungs instead of the stomach, is a primary concern. This can lead to aspiration pneumonia, a serious and potentially life-threatening infection. Furthermore, individuals with dysphagia may experience malnutrition and dehydration due to difficulty consuming enough food and fluids.
Reddit user, u/Swallowingstruggles, shared their experience:
“After my stroke, swallowing was the scariest thing. I was terrified of choking. The dysphagia diet has literally given me back my ability to enjoy food without constant fear.”
This underscores the vital role a carefully managed diet plays.
What is the Dysphagia Diet? A Layered Approach to Safe Eating
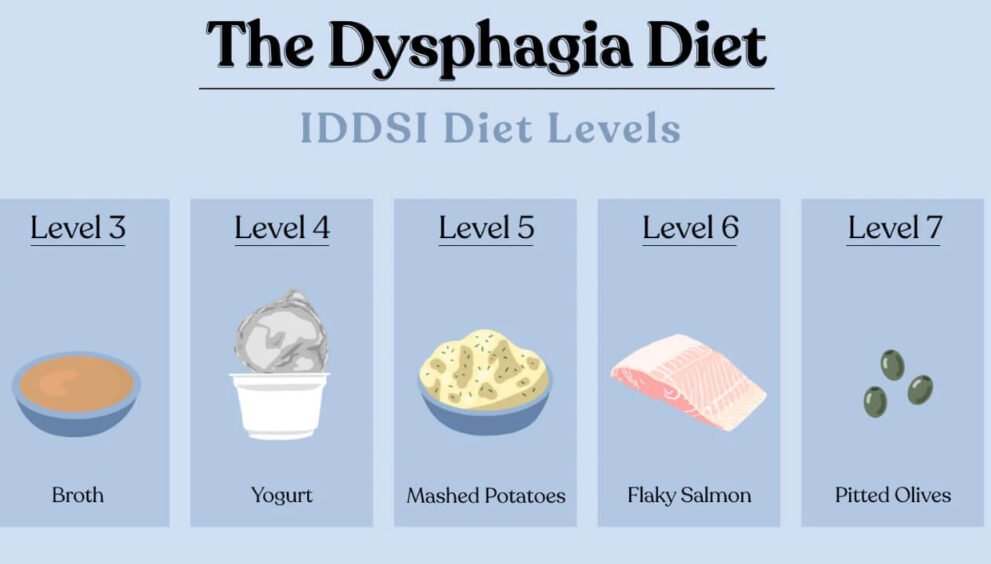
The dysphagia diet isn’t a one-size-fits-all solution. Instead, it’s a layered approach, with different levels of food textures and liquid consistencies designed to accommodate varying degrees of swallowing impairment. Speech-language pathologists (SLPs) typically assess an individual’s swallowing abilities and then recommend the appropriate diet level. Let’s break down these levels:
Solid Food Levels: A Progressive Texture Modification
The National Dysphagia Diet Task Force established a standardized system of diet levels to ensure consistency in nutritional management. These levels are progressively more challenging to swallow:
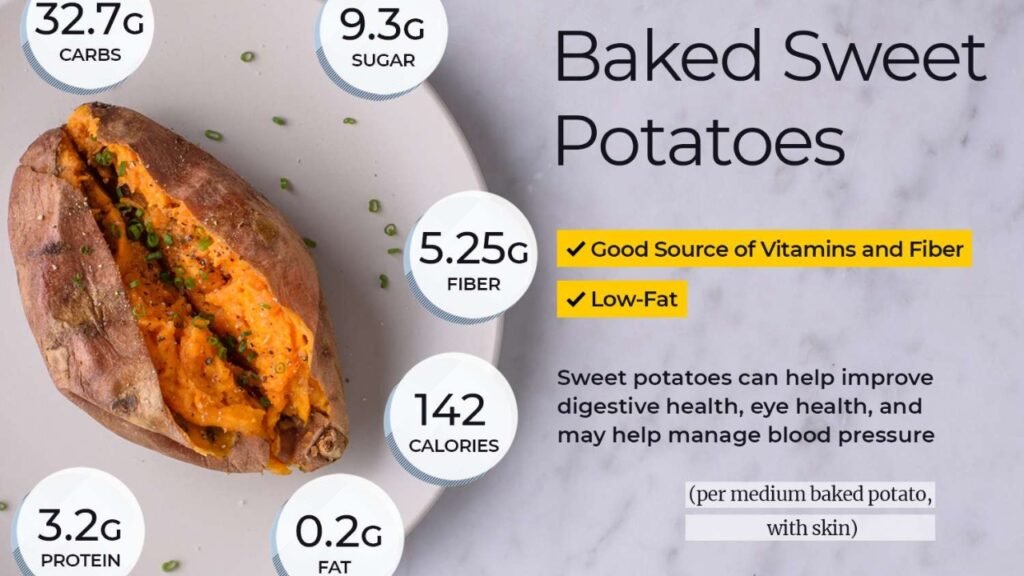
- Level 1: Pureed: This level consists of foods that are completely smooth and homogenous, with no lumps, bumps, or textures. Think applesauce, pureed sweet potatoes, or smooth yogurt. This level requires minimal chewing and is ideal for individuals with severe swallowing difficulties. For instance, pureed meats should be prepared with gravy to achieve a smooth consistency and to add some flavor.
- Level 2: Mechanically Altered (or Ground): This level includes foods that are moist, soft-textured, and easily formed into a bolus (a soft mass of food ready to be swallowed). Meats are ground, fruits and vegetables are cooked until very tender, and bread is often moistened. This level requires some chewing ability, but not much. For example, soft scrambled eggs are a good option, but fried eggs with a crispy edge are not.
- Level 3: Advanced: This level offers a transition towards a regular diet. Foods are soft and require more chewing, but still avoid hard, sticky, or crunchy items. This might include cooked pasta, tender meats, and well-cooked vegetables. However, foods like nuts, seeds, and raw vegetables are still typically excluded. An example is chicken salad without celery.
- Level 4: Regular Diet: This is a regular diet with no restrictions. This is suitable for people who are able to swallow with no difficulties.
Liquid Consistency Levels: Thin to Thick
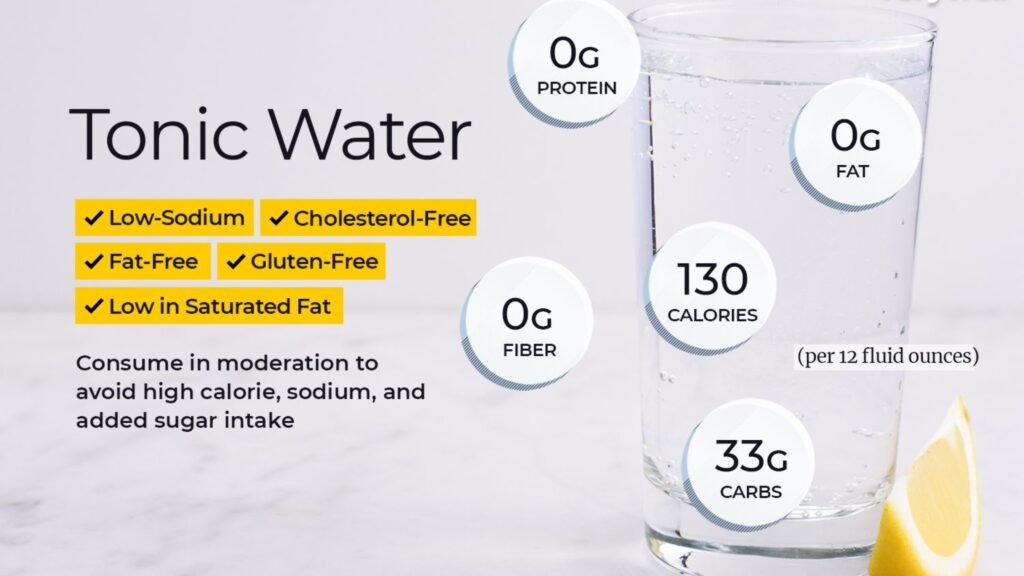
Liquid consistencies are equally important. Thin liquids, like water, can be particularly challenging for individuals with dysphagia to control, increasing the risk of aspiration. Therefore, thickening liquids is a common strategy. The levels are usually determined by an SLP.
- Thin Liquids: This includes water, juice, coffee, tea, and other beverages with a water-like consistency. These are the most difficult for some individuals with dysphagia to swallow safely.
- Nectar-Thick Liquids: This consistency is similar to that of nectar or tomato juice. It flows more slowly than thin liquids and requires more effort to swallow.
- Honey-Thick Liquids: This consistency is thicker than nectar, resembling honey. It flows slowly and requires significant effort to control in the mouth.
- Pudding-Thick Liquids: This is the thickest consistency, similar to pudding. It requires the most effort to swallow and is typically used for individuals with severe swallowing difficulties.
Thickening agents are readily available in powder or gel form, and can be added to liquids to achieve the desired consistency. However, it’s important to use these products as directed by a healthcare professional, as excessive thickening can lead to dehydration.
Implementing the Dysphagia Diet: A Practical Guide
Implementing the dysphagia diet requires careful planning and attention to detail. It’s not just about changing the textures of food; it’s about creating a safe and enjoyable eating experience. Here are some practical tips:
- Consult with a Speech-Language Pathologist (SLP): An SLP is the expert in diagnosing and managing dysphagia. They will conduct a thorough assessment of your swallowing abilities and recommend the appropriate diet level and liquid consistency.
- Read Labels Carefully: Pay close attention to the ingredients and textures of packaged foods. Avoid foods that contain small, hard pieces, like nuts or seeds, if you’re on a lower-level diet.
- Prepare Food Carefully: Use a blender, food processor, or grinder to achieve the desired consistency. Ensure that there are no lumps or chunks in pureed foods.
- Moisten Foods: Add sauces, gravies, or broths to foods to increase moisture and make them easier to swallow.
- Avoid Sticky Foods: Sticky foods, like peanut butter or caramel, can be difficult to swallow and increase the risk of choking.
- Serve Small Portions: Smaller portions are easier to manage and reduce the risk of aspiration.
- Encourage Upright Posture: Maintain an upright posture while eating and for at least 30 minutes after meals to help prevent aspiration.
- Eliminate Distractions: Create a calm and quiet eating environment to minimize distractions and promote focus on swallowing.
- Monitor for Signs of Swallowing Difficulties: Watch for signs of choking, coughing, or wet vocal quality during or after meals.
- Stay Hydrated: Dehydration can worsen swallowing difficulties. Ensure adequate fluid intake, using thickened liquids as recommended by your SLP.
Meal Planning and Recipe Ideas: Making the Dysphagia Diet Delicious
Adhering to a dysphagia diet doesn’t mean sacrificing flavor or enjoyment. With a little creativity and planning, you can create delicious and nutritious meals. Here are some recipe ideas for each diet level:
- Level 1 (Pureed):
- Pureed chicken and vegetable soup: Blend cooked chicken, carrots, celery, and broth until smooth.
- Applesauce with cinnamon: A simple and refreshing snack.
- Pureed sweet potato with a touch of maple syrup.
- Smooth yogurt with pureed berries.
- Level 2 (Mechanically Altered):
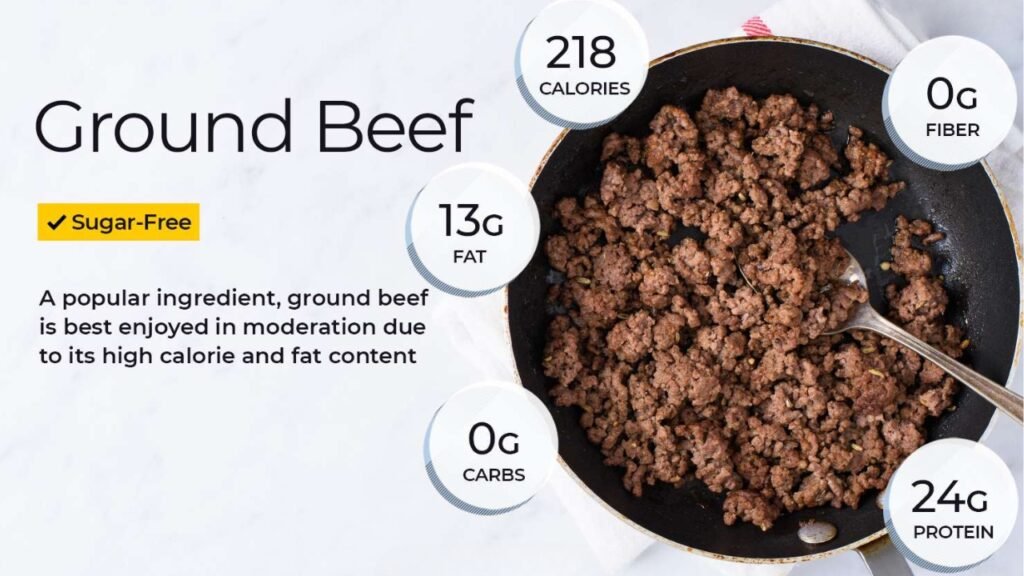
- Ground beef with mashed potatoes and gravy.
- Soft scrambled eggs with a side of pureed fruit.
- Tuna salad (made with finely shredded tuna and mayonnaise) on moistened bread.
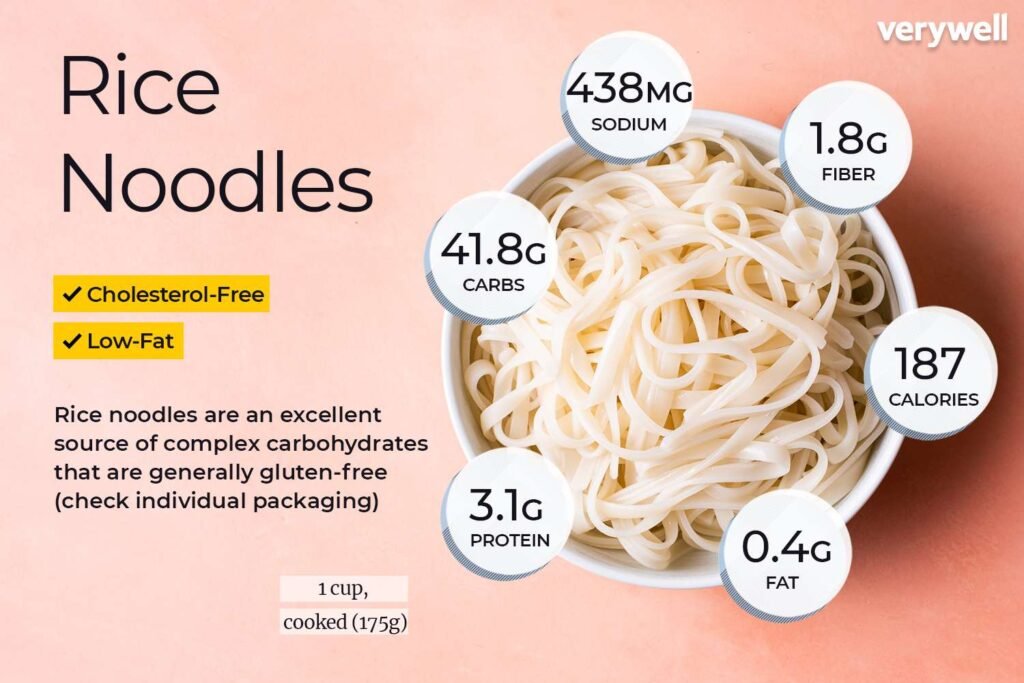
- Well-cooked pasta with a smooth tomato sauce.
- Level 3 (Advanced):
- Chicken casserole with tender vegetables and a creamy sauce.
- Macaroni and cheese (made with small pasta shapes and a smooth cheese sauce).
- Soft meatballs in marinara sauce served over pasta.
- Pancakes with syrup (ensure the pancakes are soft and not overly chewy).
The Role of Speech Therapy: Beyond Diet Modification
While diet modification is a crucial component of dysphagia management, speech therapy plays an equally important role. Speech-language pathologists provide exercises and techniques to improve swallowing strength, coordination, and safety.
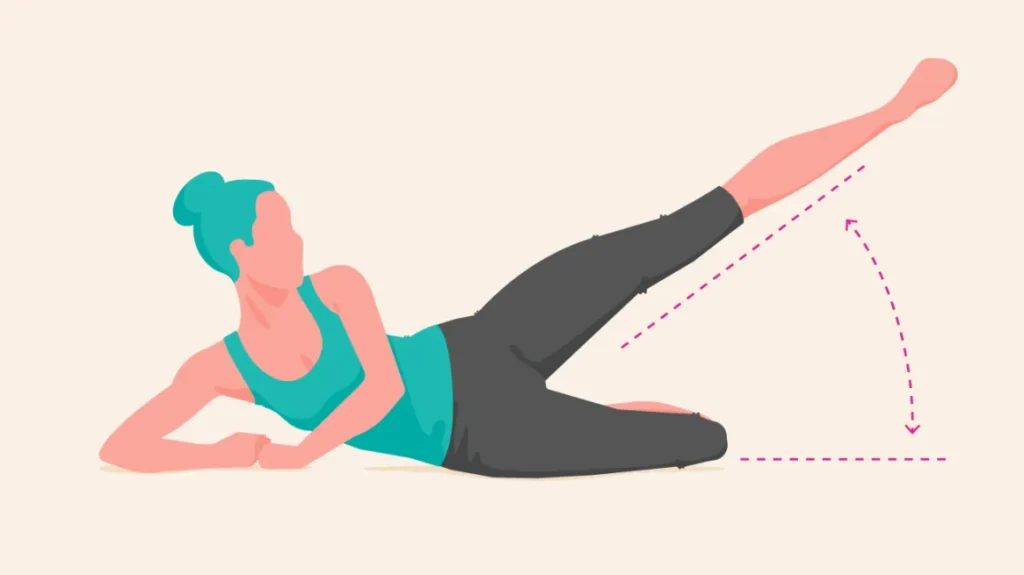
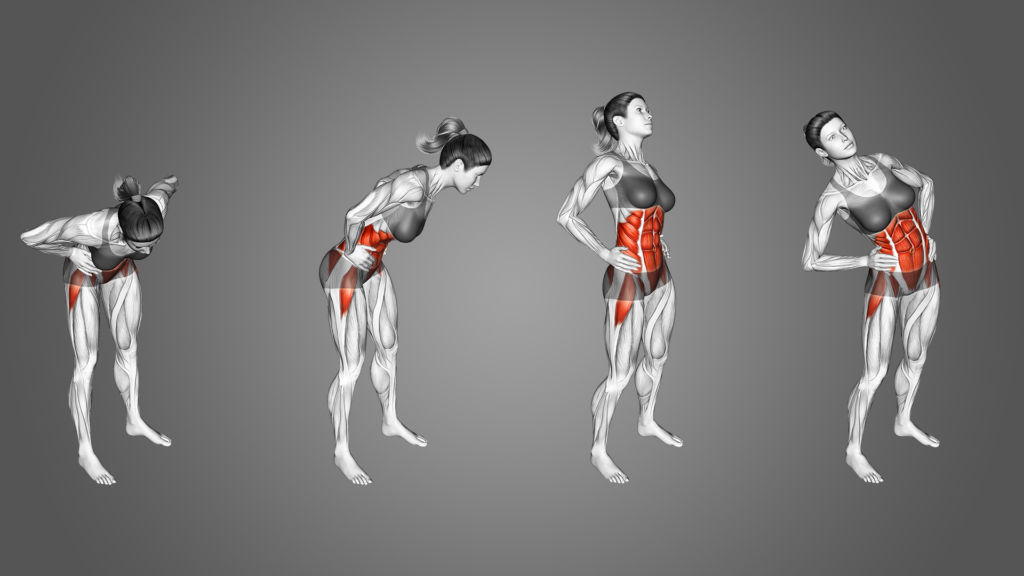
These exercises may include:
- Oral motor exercises: Strengthening the muscles of the mouth and tongue.
- Swallowing maneuvers: Techniques to protect the airway during swallowing.
- Postural adjustments: Changes in head and body position to facilitate swallowing.
“The best approach to managing dysphagia is a multidisciplinary one, including diet modifications recommended by an SLP along with exercises to retrain swallowing muscles,”
says Dr. Emily Carter, a leading expert in swallowing disorders.
“Diet is often the first step, but strengthening the oral and pharyngeal musculature will improve long term outcomes.”
The Psychological Impact of Dysphagia: Addressing Emotional Needs
Living with dysphagia can be emotionally challenging. The fear of choking, the social isolation associated with dietary restrictions, and the frustration of struggling to eat can all take a toll on mental well-being. It‘s important to acknowledge these emotional challenges and seek support when needed.
Consider these strategies to cope with the psychological impact of dysphagia:
- Join a support group: Connecting with others who have dysphagia can provide a sense of community and understanding.
- Talk to a therapist: A therapist can help you develop coping mechanisms for managing anxiety and depression related to dysphagia.
- Communicate with your family and friends: Explain your dietary restrictions and swallowing difficulties to your loved ones so they can provide support and understanding.
- Focus on what you can eat: Instead of dwelling on the foods you can’t eat, focus on the foods you can enjoy and find ways to make them delicious.
Conclusion: Finding Hope and Empowerment in Managing Dysphagia
Living with dysphagia can be challenging, but it’s important to remember that you’re not alone. With the right information, support, and strategies, you can effectively manage your swallowing difficulties and maintain a good quality of life. Remember to consult with a speech-language pathologist, follow their recommendations carefully, and advocate for your needs. While dysphagia diet modifications may seem daunting initially, they are a crucial step towards safe and comfortable eating. By embracing a proactive approach, you can find hope and empowerment in navigating the swallowing struggle and reclaim your enjoyment of food.
Blissful Bites: The Sattvic Diet Secret to Unstoppable Energy & Inner Peace!